Sleeve gastrectomy
The steps for performing sleeve gastrectomy are the same as those described for gastric bypass surgery.


Unsure what to do after surgery?
Please watch this:
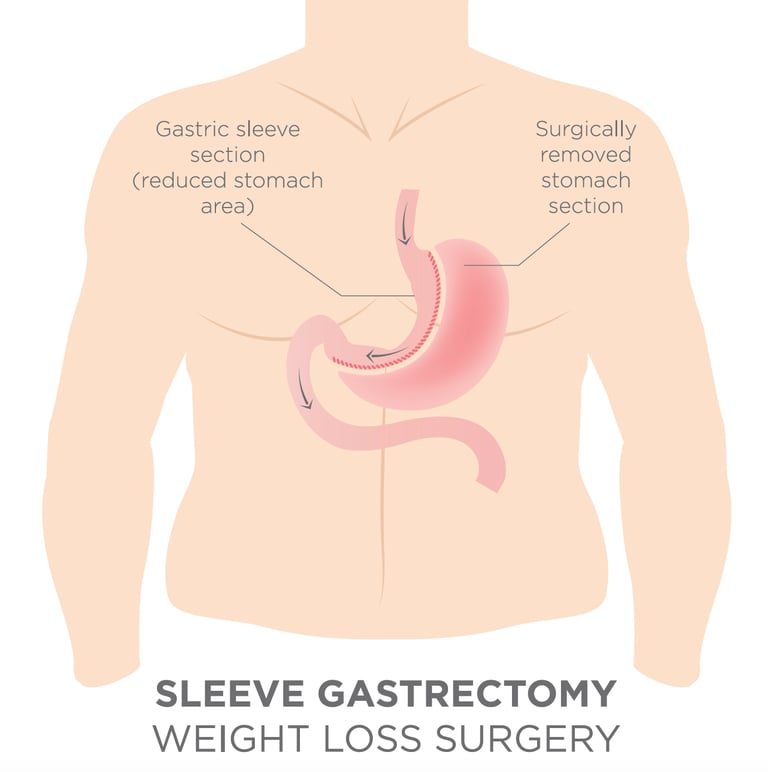
Laparoscopic Sleeve Gastrectomy (LSG), was first conceived in 2000. Over time the LSG has become the one of the most popular bariatric operations world wide. Most studies have demonstrated that the LSG is effective for weight loss, and results in improvements and even resolutions of co-morbidities like type 2 diabetes, quite similar to the effects of the Roux-en-Y gastric bypass, but with less morbidity and mortality. Procedure: The operation starts by using energy devices to take down the greater curvature of the stomach from the antrum to the Angle of His. This includes dividing various branches of the gastroepiploic vessels, close to the gastric wall of the greater curvature. Most operators will fully mobilize the fundus posteriorly, lysing the adhesions in the lesser sac and anterior to the pancreas (more so behind the antrum). The left crus is also exposed to investigate the presence of a hiatal hernia. Mr Vasas will selectively close hiatal hernias when identified and he always mobilizes the fat pad near the gastro-esophageal junction to better identify this area and staple accordingly. A bougie is introduced trans orally (34-36Fr) and positioned abutting the lesser curvature. The stapling begins 4-5 cm proximal to the pylorus and aiming lateral to the bougie. Strictures are avoided at the incisura angularis by avoiding stapling too close (or tight) to the bougie. One also has to avoid stapling the esophagus near the GE junction, as most leaks occur distal or near the GE junction. Choosing the appropriate staple height depends on gastric tissue thickness and varies according to the sex, BMI and stomach site. Wall thickness tends to decrease from distal to proximal. Appropriate compression time is necessary, especially in thick tissue. Reinforcement options include suturing or buttressing. Drainage and leak testing is always carried out.
Mr Vasas has a personal experience of more than 720 RYGB procedures (figure up to and including Oct 2022) acting as a primary surgeon, and has a rate of zero for both incidents of anastomotic leak and mortality. All his surgery data is uploaded onto the National Bariatric Surgery Registry and is publicly accessible .
The procedure of the sleeve gastrectomy
Outcomes: Most of the weight loss is achieved in the first 2 years (up to 70% excess weight loss for BMI less than 50). Weight regain and gastric pouch dilatation can be observed thereafter. At 5 years, there is a sustained weight loss in the range of 50-60% of excess weight, which equals with 30-35% of total body weight. The most feared complication of the LSG is gastric leakage (1-2%), typically occurring several days after surgery and mostly located near the GE junction. Most leaks are now treated with endoscopically placed fully covered stents, left in place for several weeks, and abscess drainage. GERD reflux is improved in 80% of patients, but in some it may remain or worsen and require prolonged medical therapy or conversion to Roux-en-Y gastric bypass. Weight loss failures can be treated with a variety of surgical options, including re-sleeve gastrectomy or conversion to Roux-en-Y gastric bypass.




